From the Journal: Distinguishing characteristics of headache in non-traumatic subarachnoid hemorrhage
Further defining the presentation of a life-threatening emergency that is commonly misdiagnosed
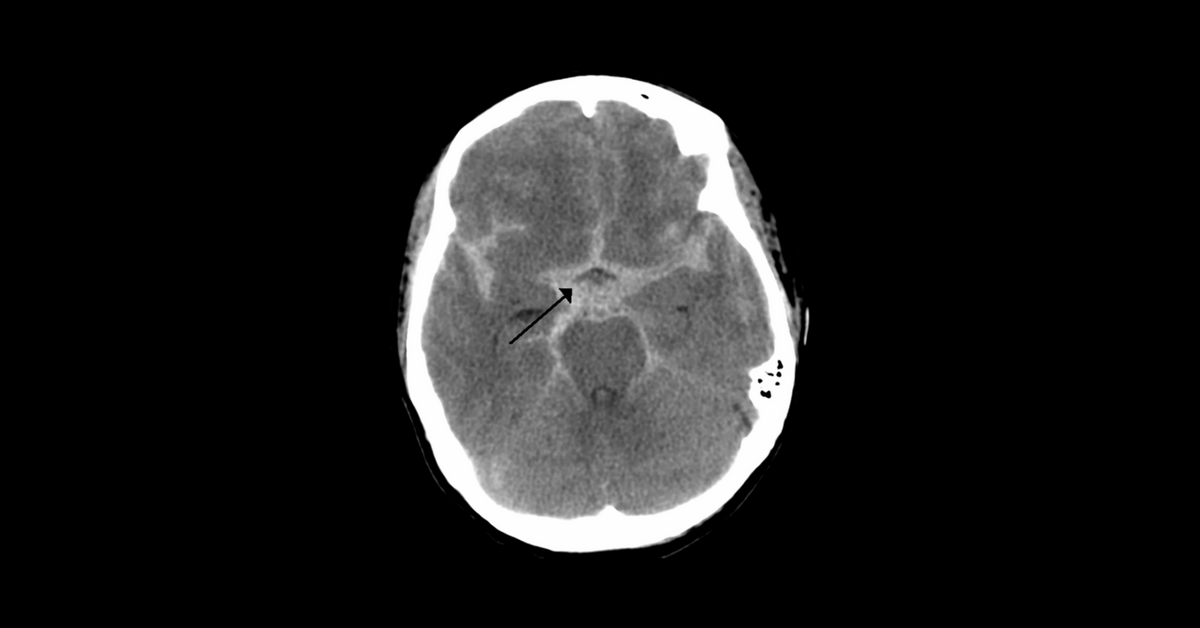
Subarachnoid hemorrhage (SAH) is a neurological emergency that occurs when there is bleeding between the brain and the tissue that covers the brain. Although it is a serious, life-threatening condition, the presentation of SAH has not been well defined by the literature. Its primary symptom—a severe, abrupt headache known as a “thunderclap” headache—can easily be mistaken for other conditions, making it difficult to assign the correct degree of urgency needed for effective treatment. A new study by Brian Mac Grory, MD, Linh Vu, MD, Shawna Cutting, MD, Evadne Marcolini, MD, FACEP, FAAEM, Christopher Gottschalk, MD, FAHS, and David Greer, MD, MA, FCCM, FAHA, FNCS, FAAN, is the first examine in detail the clinical characteristics of the presenting headache in SAH in the hopes of providing a better diagnostic framework.
The prospective, observational study, published in Headache under the title “Distinguishing characteristics of headache in non-traumatic subarachnoid hemorrhage”, took place at a tertiary academic medical center specializing in neurological care where 158 subjects were enrolled. The patients participating in the study were enrolled through the emergency department and the neurosciences intensive care unit, where it was determined whether or not their headache was caused by SAH. Then, the clinical features of the headache were recorded to determine possible characteristics.
Of the 158 patients, 20 had headache caused by SAH. Researchers found that 65% of patients with SAH reported that their headache peaked within 1 second of onset, compared with only 10% of those headache not caused by SAH. Other notable distinguishing features included occipital location (55% in the SAH group vs. 22% in the non-SAH group, P<0.001), “stabbing” quality (35% in the SAH group vs. 5% in the non-SAH group, P<0.001) and the presence of a prior headache (50% in the SAH group vs. 83% in the non-SAH group, p=0.002).
The distinct differences observed in the timeline, location, “stabbing” quality and presence of prior headache between the SAH and non-SAH group suggests that the clinical features of headache with SAH are distinct from those associated with other headache syndromes. In most emergency department settings, patients are triaged by urgency. Because SAH does not present visibly, it is important to provide as much information as possible for individuals at risk of SAH so they are equipped to properly advocate for their care. The new distinctions uncovered in this study can aid patients and clinicians in accurately diagnosing SAH, improving their ability to respond appropriately and provide life-saving care.
The American Headache Society is committed to keeping its members up to date on the most innovative and meaningful advancements in the realm of headache medicine. One of many initiatives to support that mission is our publication of Headache: The Journal of Head and Face Pain, published ten times per year, which highlights the latest findings in the realm of headache medicine research. Our “From the Journal” series offers a preview of some of the groundbreaking work detailed in Headache. Enjoy access to the full catalogue of content plus a print subscription included with an American Headache Society Membership. Click here to become a member today.


